Gestational age
In obstetrics, gestational age is a measure of the age of a pregnancy taken from the beginning of the woman's last menstrual period (LMP),[1] or the corresponding age of the gestation as estimated by a more accurate method, if available. Such methods include adding 14 days to a known duration since fertilization (as is possible in in vitro fertilization), or by obstetric ultrasonography. The popularity of using this measure of pregnancy is largely due to convenience: menstruation is usually noticed, while there is generally no convenient way to discern when fertilization or implantation occurred.
Gestational age is contrasted with fertilization age, which takes the date of fertilization as the start date of gestation. There are different approaches to defining the start of a pregnancy. This definition is unusual in that it describes women as becoming "pregnant" about two weeks before they even had sex. The definition of pregnancy and the calculation of gestational age are also relevant in the context of the abortion debate and the philosophical debate over the beginning of human personhood.
Methods
[edit]According to American College of Obstetricians and Gynecologists, the main methods to calculate gestational age are:[2]
- Directly calculating the days since the beginning of the last menstrual period
- Early obstetric ultrasound, comparing the size of an embryo or fetus to that of a reference group of pregnancies of known gestational age (such as calculated from last menstrual periods) and using the mean gestational age of other embryos or fetuses of the same size. If the gestational age as calculated from an early ultrasound is contradictory to the one calculated directly from the last menstrual period, it is still the one from the early ultrasound that is used for the rest of the pregnancy.[2]
- In case of in vitro fertilization, calculating days since oocyte retrieval or co-incubation and adding 14 days.[3]
Gestational age can also be estimated by calculating days from ovulation if it was estimated from related signs or ovulation tests, and adding 14 days by convention.[4]
A more complete listing of methods is given in following table:[5]
| Method of estimating gestational age | Variability (2 standard deviations)[5] |
|---|---|
| Days from oocyte retrieval or co-incubation in in vitro fertilisation + 14 days | ±1 day |
| Days from estimated ovulation in ovulation induction + 14 days | ±3 days |
| Days from artificial insemination + 14 days | ±3 days |
| Days from known single sexual intercourse + 14 days | ±3 days |
| Days from estimated ovulation by basal body temperature record + 14 days | ±4 days |
| First-trimester physical examination | ±2 weeks |
| Second-trimester physical examination | ±4 weeks |
| Third-trimester physical examination | ±6 weeks |
| First-trimester obstetric ultrasonography (crown-rump length) | ±8% of the estimate |
| Second-trimester obstetric ultrasonography (head circumference, femur length) | ±8% of the estimate |
| Third-trimester obstetric ultrasonography (head circumference, femur length) | ±8% of the estimate |
As a general rule, the official gestational age should be based on the actual beginning of the last menstrual period, unless any of the above methods gives an estimated date that differs more than the variability for the method, in which case the difference cannot probably be explained by that variability alone.[5] For example, if there is a gestational age based on the beginning of the last menstrual period of 9.0 weeks, and a first-trimester obstetric ultrasonography gives an estimated gestational age of 10.0 weeks (with a 2 SD variability of ±8% of the estimate, thereby giving a variability of ±0.8 weeks), the difference of 1.0 weeks between the tests is larger than the 2 SD variability of the ultrasonography estimate, indicating that the gestational age estimated by ultrasonography should be used as the official gestational age.[5]
Once the estimated due date (EDD) is established, it should rarely be changed, as the determination of gestational age is most accurate earlier in the pregnancy.[6]
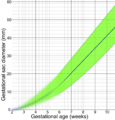
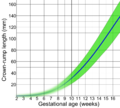
Assessment of gestational age can be made based on selected head and trunk parameters.[7] Following are diagrams for estimating gestational age from obstetric ultrasound, by various target parameters:
-
By gestational sac diameter
-
By crown-rump length (CRL)
-
By biparietal diameter (BPD)
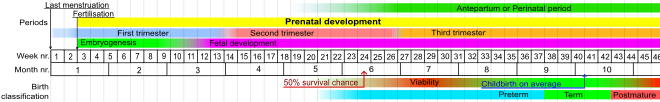
Comparison to fertilization age
[edit]The fertilization or conceptional age (also called embryonic age and later fetal age) is the time from the fertilization. It usually occurs within a day of ovulation, which, in turn, occurs on average 14.6 days after the beginning of the preceding menstruation (LMP).[8] There is also considerable variability in this interval, with a 95% prediction interval of the ovulation of 9 to 20 days after menstruation even for an average woman who has a mean LMP-to-ovulation time of 14.6.[9] In a reference group representing all women, the 95% prediction interval of the LMP-to-ovulation is 8.2 to 20.5 days.[8] The actual variability between gestational age as estimated from the beginning of the last menstrual period (without the use of any additional method mentioned in previous section) is substantially larger because of uncertainty which menstrual cycle gave rise to the pregnancy. For example, the menstruation may be scarce enough to give the false appearance that an earlier menstruation gave rise to the pregnancy, potentially giving an estimated gestational age that is approximately one month too large. Also, vaginal bleeding occurs during 15–25% of first trimester pregnancies,[10] and may be mistaken as menstruation, potentially giving an estimated gestational age that is too low.
Uses
[edit]Gestational age is used for example for:[citation needed]
- The events of prenatal development, which usually occur at specific gestational ages. Hence, the gestational timing of a fetal toxin exposure, fetal drug exposure or vertically transmitted infection can be used to predict the potential consequences to the fetus.
- Estimated date of delivery
- Scheduling prenatal care
- Estimation of fetal viability
- Calculating the results of various prenatal tests, (for example, in the triple test).
- Birth classification into for example preterm, term or postterm.
- Classification of infant deaths and stillbirths
- Postnatally (after birth) to estimate various risk factors

Estimation of due date
[edit]
The mean pregnancy length has been estimated to be 283.4 days of gestational age as timed from the first day of the last menstrual period and 280.6 days when retrospectively estimated by obstetric ultrasound measurement of the fetal biparietal diameter (BPD) in the second trimester.[12] Other algorithms take into account other variables, such as whether this is the first or subsequent child, the mother's race, age, length of menstrual cycle, and menstrual regularity. In order to have a standard reference point, the normal pregnancy duration is assumed by medical professionals to be 280 days (or 40 weeks) of gestational age. Furthermore, actual childbirth has only a certain probability of occurring within the limits of the estimated due date. A study of singleton live births determined that childbirth has a standard deviation of 14 days when gestational age is estimated by first-trimester ultrasound and 16 days when estimated directly by last menstrual period.[11]
The most common system used among healthcare professionals is Naegele's rule, which estimates the expected date of delivery (EDD) by adding a year, subtracting three months, and adding seven days to the first day of a woman's last menstrual period (LMP) or corresponding date as estimated from other means.
Medical fetal viability
[edit]There is no sharp limit of development, gestational age, or weight at which a human fetus automatically becomes viable.[13] According to studies between 2003 and 2005, 20 to 35 percent of babies born at 23 weeks of gestation survive, while 50 to 70 percent of babies born at 24 to 25 weeks, and more than 90 percent born at 26 to 27 weeks, survive.[14] It is rare for a baby weighing less than 500 g (17.6 ounces) to survive.[13] A baby's chances for survival increases 3–4% per day between 23 and 24 weeks of gestation and about 2–3% per day between 24 and 26 weeks of gestation. After 26 weeks the rate of survival increases at a much slower rate because survival is high already.[15] Prognosis depends also on medical protocols on whether to resuscitate and aggressively treat a very premature newborn, or whether to provide only palliative care, in view of the high risk of severe disability of very preterm babies.[16]
| Completed weeks of gestation at birth | 21 and less | 22 | 23 | 24 | 25 | 26 | 27 | 30 | 34 |
|---|---|---|---|---|---|---|---|---|---|
| Chance of survival[15] | <1%[17] | 0–10% | 10–35% | 40–70% | 50–80% | 80–90% | >90% | >95% | >98% |
Birth classification
[edit]Using gestational age, births can be classified into broad categories:
| Gestational Age in Weeks | Classification |
|---|---|
| < 37 0/7 | Preterm |
| 34 0/7 - 36 6/7 | Late preterm[18] |
| 37 0/7 - 38 6/7 | Early Term[19] |
| 39 0/7 - 40 6/7 | Full Term[19] |
| 41 0/7 - 41 6/7 | Late Term[19] |
| > 42 0/7 | Postterm |
Using the LMP (last menstrual period) method, a full-term human pregnancy is considered to be 40 weeks (280 days), though pregnancy lengths between 38 and 42 weeks are considered normal. A fetus born prior to the 37th week of gestation is considered to be preterm. A preterm baby is likely to be premature and consequently faces increased risk of morbidity and mortality. An estimated due date is given by Naegele's rule.
According to the WHO, a preterm birth is defined as "babies born alive before 37 weeks of pregnancy are completed."[20] According to this classification, there are three sub-categories of preterm birth, based on gestational age: extremely preterm (fewer than 28 weeks), very preterm (28 to 32 weeks), moderate to late preterm (32 to 37 weeks).[20] Various jurisdictions may use different classifications.
In classifying perinatal deaths, stillbirths and infant deaths
[edit]For most of the 20th century, official definitions of a live birth and infant death in the Soviet Union and Russia differed from common international standards, such as those established by the World Health Organization in the latter part of the century.[21][22] Babies who were fewer than 28 weeks of gestational age, or weighed fewer than 1000 grams, or fewer than 35 cm in length – even if they showed some sign of life (breathing, heartbeat, voluntary muscle movement) – were classified as "live fetuses" rather than "live births." Only if such newborns survived seven days (168 hours) were they then classified as live births. If, however, they died within that interval, they were classified as stillbirths. If they survived that interval but died within the first 365 days they were classified as infant deaths.
More recently, thresholds for "fetal death" continue to vary widely internationally, sometimes incorporating weight as well as gestational age. The gestational age for statistical recording of fetal deaths ranges from 16 weeks in Norway, to 20 weeks in the US and Australia, 24 weeks in the UK, and 26 weeks in Italy and Spain.[23][24][25]
The WHO defines the perinatal period as "The perinatal period commences at 22 completed weeks (154 days) of gestation and ends seven completed days after birth."[26] Perinatal mortality is the death of fetuses or neonates during the perinatal period. A 2013 study found that "While only a small proportion of births occur before 24 completed weeks of gestation (about 1 per 1000), survival is rare and most of them are either fetal deaths or live births followed by a neonatal death."[23]
Postnatal use
[edit]Gestational age (as well as fertilization age) is sometimes used postnatally (after birth) to estimate various risk factors. For example, it is a better predictor than postnatal age for risk of intraventricular hemorrhage in premature babies treated with extracorporeal membrane oxygenation.[27]
Factors affecting pregnancy length
[edit]Child's gestational age at birth (pregnancy length) is associated with various likely causal maternal non-genetic factors: stress during pregnancy,[28] age, parity, smoking, infection and inflammation, BMI. Also, preexisting maternal medical conditions with genetic component, e.g., diabetes mellitus type 1, systemic lupus erythematosus, anaemia. Parental ancestral background (race) also plays a role in pregnancy duration. Gestational age at birth is on average shortened by various pregnancy aspects: twin pregnancy, prelabor rupture of (fetal) membranes, pre-eclampsia, eclampsia, intrauterine growth restriction.[29] The ratio between fetal growth rate and uterine size (reflecting uterine distension) is suspected to partially determine the pregnancy length.[30]
Heritability of pregnancy length
[edit]Family-based studies showed that gestational age at birth is partially (25–40%) determined by genetic factors.[31]
See also
[edit]- Pregnancy
- Maternity
- Prenatal development
- Gestation periods in mammals
- Abortion law
- Reproductive rights
- Fetal rights
References
[edit]- ^ "Gestational age: MedlinePlus Medical Encyclopedia". medlineplus.gov.
- ^ a b Obstetric Data Definitions Issues and Rationale for Change - Gestational Age & Term Archived 2013-11-06 at the Wayback Machine from Patient Safety and Quality Improvement at American Congress of Obstetricians and Gynecologists. Created November 2012.
- ^ Tunon, K.; Eik-Nes, S. H.; Grøttum, P.; Von Düring, V.; Kahn, J. A. (2000). "Gestational age in pregnancies conceived after in vitro fertilization: A comparison between age assessed from oocyte retrieval, crown-rump length and biparietal diameter". Ultrasound in Obstetrics and Gynecology. 15 (1): 41–46. doi:10.1046/j.1469-0705.2000.00004.x. PMID 10776011. S2CID 20029116.
- ^ Robinson, H. P.; Fleming, J. E. E. (1975). "A Critical Evaluation of Sonar "crown-Rump Length" Measurements". BJOG: An International Journal of Obstetrics and Gynaecology. 82 (9): 702–10. doi:10.1111/j.1471-0528.1975.tb00710.x. PMID 1182090. S2CID 31663686.
- ^ a b c d A Simple Solution to Dating Discrepancies: The Rule of Eights Hunter, L. A. (2009). "Issues in Pregnancy Dating: Revisiting the Evidence". Journal of Midwifery & Women's Health. 54 (3): 184–190. doi:10.1016/j.jmwh.2008.11.003. PMID 19410210.
- ^ "Committee Opinion No 611". Obstetrics & Gynecology. 124 (4): 863–866. 2014. doi:10.1097/01.AOG.0000454932.15177.be. PMID 25244460.
- ^ Kędzia, Alicja; Woźniak, Jowita; Ziajkiewicz, Marcin; Dudek, Krzysztof; Derkowski, Wojciech (2009). "Foetal age assessment on the basis of selected parameters of head and trunk". The computer-aided scientific research. Vol. 16. Wrocław Scientific Society. pp. 241–246. ISBN 978-83-7374-060-0.
- ^ a b Geirsson RT (May 1991). "Ultrasound instead of last menstrual period as the basis of gestational age assignment". Ultrasound Obstet Gynecol. 1 (3): 212–9. doi:10.1046/j.1469-0705.1991.01030212.x. PMID 12797075. S2CID 29063110.
- ^ Derived from a standard deviation in this interval of 2.6, as given in: Fehring RJ, Schneider M, Raviele K (2006). "Variability in the phases of the menstrual cycle". J Obstet Gynecol Neonatal Nurs. 35 (3): 376–84. doi:10.1111/j.1552-6909.2006.00051.x. PMID 16700687. S2CID 30317703.
- ^ Snell, BJ (Nov–Dec 2009). "Assessment and management of bleeding in the first trimester of pregnancy". Journal of Midwifery & Women's Health. 54 (6): 483–91. doi:10.1016/j.jmwh.2009.08.007. PMID 19879521.
- ^ a b Hoffman, Caroline S.; Messer, Lynne C.; Mendola, Pauline; Savitz, David A.; Herring, Amy H.; Hartmann, Katherine E. (2008). "Comparison of gestational age at birth based on last menstrual period and ultrasound during the first trimester". Paediatric and Perinatal Epidemiology. 22 (6): 587–596. doi:10.1111/j.1365-3016.2008.00965.x. ISSN 0269-5022. PMID 19000297.
- ^ Kieler, H; Axelsson, O; Nilsson, S; Waldenströ, U (1995). "The length of human pregnancy as calculated by ultrasonographic measurement of the fetal biparietal diameter". Ultrasound in Obstetrics and Gynecology. 6 (5): 353–7. doi:10.1046/j.1469-0705.1995.06050353.x. PMID 8590208. S2CID 39447672.
- ^ a b Moore, Keith and Persaud, T. The Developing Human: Clinically Oriented Embryology, p. 103 (Saunders 2003).
- ^ March of Dimes --> Neonatal Death Archived 2014-10-24 at the Wayback Machine Retrieved on November 10, 2014. In turn citing:
- Tyson JE, Parikh NA, Langer J, Green C, Higgins RD (April 2008). "Intensive care for extreme prematurity--moving beyond gestational age". N. Engl. J. Med. 358 (16): 1672–81. doi:10.1056/NEJMoa073059. PMC 2597069. PMID 18420500.
- Luke B, Brown MB (December 2006). "The changing risk of infant mortality by gestation, plurality, and race: 1989-1991 versus 1999-2001". Pediatrics. 118 (6): 2488–97. doi:10.1542/peds.2006-1824. PMC 3623686. PMID 17142535.
- The American College of Obstetricians and Gynecologists (September 2002). "ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrcian-Gynecologists: Number 38, September 2002. Perinatal care at the threshold of viability". Obstet Gynecol. 100 (3): 617–24. doi:10.1016/S0029-7844(02)02260-3. PMID 12220792.
- ^ a b (). What are the chances that my baby will survive?. [ONLINE] Available at: http://www.spensershope.org/chances_for_survival.htm Archived 2018-08-09 at the Wayback Machine. [Last Accessed 14 November 2012].
- ^ Verlato, Giovanna; Gobber, Daniela; Drago, Donatella; Chiandetti, Lino; Drigo, Paola; Working Group of Intensive Care in the Delivery Room of Extremely Premature Newborns (2016). "Guidelines for Resuscitation in the Delivery Room of Extremely Preterm Infants". Journal of Child Neurology. 19 (1): 31–4. doi:10.1177/088307380401900106011. PMID 15032380. S2CID 20200767.
- ^ "World's most premature baby defies sub-1% survival odds to break record". Guinness World Records. 10 November 2021. Retrieved 2022-03-15.
- ^ Late-Preterm Infants Archived 2012-05-02 at the Wayback Machine ACOG Committee Opinion 404
- ^ a b c Ob-Gyns Redefine Meaning of "Term Pregnancy" Archived 2017-05-03 at the Wayback Machine, from American College of Obstetricians and Gynecologists. October 22, 2013
- ^ a b "Preterm birth".
- ^ Anderson, Barbara A; Silver, Brian D (1986). "Infant Mortality in the Soviet Union: Regional Differences and Measurement Issues". Population and Development Review. 12 (4): 705–38. doi:10.2307/1973432. JSTOR 1973432.
- ^ Anderson, Barbara A.; Silver, Brian D. (1994). "The Geodemography of Infant Mortality in the Soviet Union, 1950-1990". PSC Research Report No. 94-316: 8.
- ^ a b Mohangoo, Ashna D; Blondel, Béatrice; Gissler, Mika; Velebil, Petr; MacFarlane, Alison; Zeitlin, Jennifer (2013). "International Comparisons of Fetal and Neonatal Mortality Rates in High-Income Countries: Should Exclusion Thresholds Be Based on Birth Weight or Gestational Age?". PLOS ONE. 8 (5): e64869. Bibcode:2013PLoSO...864869M. doi:10.1371/journal.pone.0064869. PMC 3658983. PMID 23700489.
- ^ Li, Z; Zeki, R; Hilder, L; Sullivan, EA (2012). "Australia's Mothers and Babies 2010". Perinatal statistics series no. 27. Cat. no. PER 57. Australian Institute of Health and Welfare National Perinatal Statistics Unit, Australian Government. Retrieved 4 July 2013.
- ^ Royal College of Obstetricians; Gynaecologists UK (April 2001). "Further Issues Relating to Late Abortion, Fetal Viability and Registration of Births and Deaths". Royal College of Obstetricians and Gynaecologists UK. Archived from the original on 5 November 2013. Retrieved 4 July 2013.
- ^ [1][full citation needed]
- ^ Jobe, Alan H (2004). "Post-conceptional age and IVH in ECMO patients". The Journal of Pediatrics. 145 (2): A2. doi:10.1016/j.jpeds.2004.07.010.
- ^ Dole, N.; Savitz, D. A.; Hertz-Picciotto, I.; Siega-Riz, A. M.; McMahon, M. J.; Buekens, P. (2003-01-01). "Maternal stress and preterm birth". American Journal of Epidemiology. 157 (1): 14–24. doi:10.1093/aje/kwf176. ISSN 0002-9262. PMID 12505886.
- ^ Goldenberg, Robert L.; Culhane, Jennifer F.; Iams, Jay D.; Romero, Roberto (2008-01-05). "Epidemiology and causes of preterm birth". Lancet. 371 (9606): 75–84. doi:10.1016/S0140-6736(08)60074-4. ISSN 1474-547X. PMC 7134569. PMID 18177778.
- ^ Bacelis, Jonas; Juodakis, Julius; Waldorf, Kristina M. Adams; Sengpiel, Verena; Muglia, Louis J.; Zhang, Ge; Jacobsson, Bo (2018-10-01). "Uterine distention as a factor in birth timing: retrospective nationwide cohort study in Sweden". BMJ Open. 8 (10): e022929. doi:10.1136/bmjopen-2018-022929. ISSN 2044-6055. PMC 6252709. PMID 30385442.
- ^ Clausson, Britt; Lichtenstein, Paul; Cnattingius, Sven (2000). "Genetic influence on birthweight and gestational length determined by studies in offspring of twins". BJOG. 107 (3): 375–81. doi:10.1111/j.1471-0528.2000.tb13234.x. PMID 10740335. S2CID 43470321.